History
A midwife calls the neonatal intensive care unit asking for an urgent review of a baby born 10 minutes ago. At delivery they thought it was a boy and said this to the parents. Now they are not so sure because although the baby appears to have a penis, there is no obvious scrotum and they cannot feel the testes. The baby seems otherwise normal and there was nothing remarkable about the pregnancy. It is the parents’ first child.
Examination
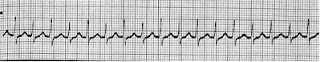
There are no dysmorphic features and examination of the cardiovascular, respiratory and abdominal systems are normal. The weight is 3.1 kg. There is a 1.5 cm phallus
(normal in term newborn males 2.5 cm) with a single perineal opening at the base of the phallus
"which is a penis-shaped object such as a dildo, or a mimetic image of an erect penis". There is pigmentation of the labioscrotal folds, which are fused with no obvious vaginal opening. There are no palpable gonads, including in the inguinal canals. The anus is normally positioned. The baby’s external genitalia can be seen in the figure below.
Questions Are :- Is this a boy or a girl?
- What is the most likely diagnosis and the differential?
- What investigations are needed?
Case Discussion
At this stage, no one can or should say whether this baby is a boy or a girl. It is imperative not to guess as it could be either a virilized female (a normal girl exposed in utero to excess androgens) or an undervirilized male. Disorders of sexual differentiation (DSD) are a medical and social emergency and families find it exceptionally difficult not knowing the sex of their baby. Pending urgent tests they should not name the baby or register the birth.
In the absence of palpable gonads, but with evidence of virilization with a small phallus and pigmentation, it is most likely that this is a virilized female. Much the commonest aetiology is congenital adrenal hyperplasia (CAH).
If the baby is an undervirilized male,there is a much larger differential, including disorders of gonadotrophin production (e.g. Kallman syndrome), defects of testosterone synthesis and end-organ insensitivity due to androgen receptor abnormalities. With very severe undervirilization, it is possible that the sex of rearing should be female. Such babies need urgent referral to a specialist centre with a team of endocrinologists, urologists, geneticists and psychologists.
Congenital adrenal hyperplasia is a group of autosomal recessive inborn errors of metabolism (IEM) (therefore commoner if parents are consanguineous), within the adrenal steroidogenic pathways that produce mineralocorticoids (aldosterone), glucocorticoids (cortisol) and androgens (testosterone). 95 % of cases are due to 21-hydroxylase deficiency (21-OHD) that catalyses late steps in the first two pathways. The consequences are the same as for any IEM – deficiency of the end product, continued drive through the pathway, build-up of precursors and diversion down alternative pathways. Lack of cortisol causes hypoglycaemia and a poor stress response. Elevated precursors divert to the androgen pathway and testosterone virilizes both male and female fetuses. Most babies are also aldosterone-deficient. Those missed at birth (usually virilized boys) classically present in the second week of life with a salt-wasting (Addisonian) crisis – vomiting and shocked with severe hyponatraemia, hyperkalaemia and acidosis.
Patients with 21-OHD need lifelong steroid replacement, initially with hydrocortisone and fludrocortisone (a mineralocorticoid analogue), and endocrine monitoring.
The timing of any surgery to reduce clitoromegaly and create a vaginal orifice is controversial.
*Investigations in the first few days consider the differential diagnosis and monitor for complications:
• karyotype – result in 48 hours if laboratory warned
• pelvic and abdominal ultrasound – extremely helpful and immediately available
• 17-hydroxyprogesterone – sent after 48 hours as raised in all newborns
• full male hormone profile
• urine steroid profile – confirms site of block in steroidogenic pathway
• electrolytes and glucose – from day 2; monitor bedside glucose
• plasma renin activity – best estimation of salt status.
KEY POINTS
1- Never guess the sex of a newborn baby with abnormal genitalia.
2- Virilization of a female infant is almost always congenital adrenal hyperplasia due to 21-hydroxylase deficiency.